The gene therapy developed by Vertex Pharmaceuticals and CRISPR Therapeutics for the treatment of beta thalassemia, requiring regular blood transfusions in patients aged 12 and older, has received approval from the US health regulator, as announced by Vertex on Tuesday.
This approval marks the second for the therapy, known as Casgevy, following its clearance in December for the treatment of sickle cell disease, another inherited blood disorder.
The Food and Drug Administration’s approval was granted over two months earlier than the anticipated action date of March 30.
Casgevy, designed for administration through authorized treatment centers experienced in stem cell transplantation, is set to be accessible in the United States early this year at a listed price of $2.2 million for both approved indications, according to Vertex’s email response.
Analyst Hartaj Singh from Oppenheimer anticipates a gradual introduction of the therapy, estimating combined peak sales of approximately $400 million.
First CRISPR Therapy Approved for Beta Thalassemia
Casgevy achieves the distinction of being the initial treatment, leveraging the Nobel Prize-winning CRISPR gene editing technology, to attain approval for transfusion-dependent beta thalassemia (TDT) in the United States.
CRISPR, pioneered by Jennifer Doudna and CRISPR Therapeutics co-founder Emmanuelle Charpentier, employs molecular “scissors” to excise defective segments of genes, allowing them to be either disabled or replaced with new strands of normal DNA.
In 2022, bluebird bio’s Zynteglo, a rival cell-based gene therapy, secured FDA approval for treating adult and pediatric patients with TDT and set a pricing record at $2.8 million.
What is Beta-thalassemia?
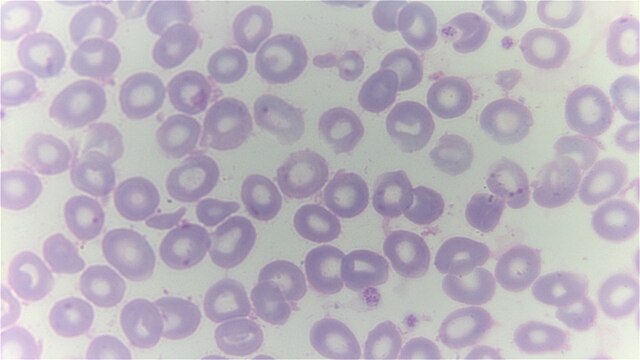
Beta thalassemia is a condition characterized by insufficient production of hemoglobin, the molecule responsible for carrying oxygen in the blood.
This deficiency results in anemia, leading to feelings of weakness, fatigue, and breathlessness. Beta thalassemia can contribute to a shortened lifespan.
Historically, the condition has been addressed through regular blood transfusions. However, frequent transfusions may lead to a complication known as iron overload syndrome, necessitating additional management strategies.
Boston Children’s Hospital estimates that at least 1,200 individuals in the United States have thalassemia severe enough to require blood transfusions for management.
